How does Hospital Billing actually work?
The Process (for insured patients)
The hospital billing process can be somewhat confusing. It's very complex, and most people - those who don't work in healthcare, are unaware of the various stages involved. Here's a simple breakdown of what happens behind the scenes, before you get your bill.
Once a hospital visit occurs, you'll be asked for your insurance card, and to fill out some paperwork. The services are rendered, and a few weeks later you receive an "Explanation of Benefits" and a bill from the hospital. How did this happen?
During or after your visit, a doctor, nurse or scribe writes notes about your visit in an Electronic Medical record (EMR) or Electronic Health Record (EHR). These notes are then translated by a certified medical coder into a claim, that the hospital then sends to your insurer, so the hospital can be paid for the services.
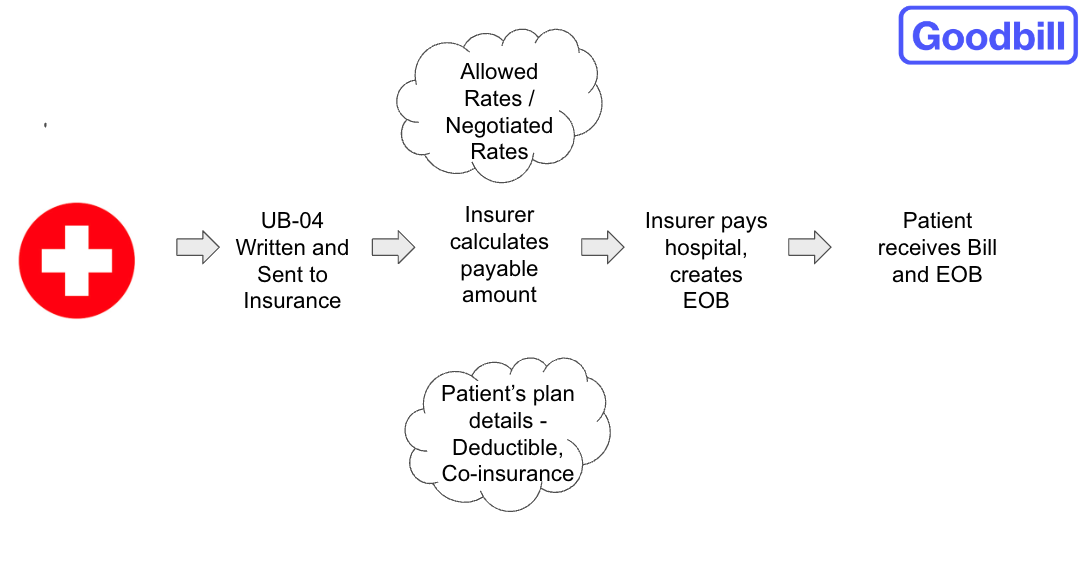
The claim is sent in the form of a UB-04 form - this is also the form that Goodbill commonly uses to review all the charges on your bill. It includes revenue codes, CPT/HCPCS codes, and every single line item from the bill is accounted for.
The insurer receives and adjudicates the claim. Adjudication involves things like making the decisions of what to cover, what to not cover, adjusting down to negotiated rates, checking for accuracy, how much to pay, and how much the patient should pay (what’s called cost sharing).
The insurer then pays their portion of the bill, and generates an Explanation of Benefits which is sent to the patient. This outlines what the insurer has covered, and what is left to the patient responsibility. The patient then receives the EOB and the hospital is paid by the insurer, after which the hospital sends the bill outlining the patient responsibility for the charges, to the patient.
Hospital Bills vs Professional Bills
Often, a patient will receive multiple bills from one hospital visit. Goodbill works with the hospital bills - these are the charges for the facility, equipment and procedures from the hospital. Professional bills are usually doctor's charges, but could also be charges from third-party radiology, anesthesia, laboratory, or transport companies. The hospital portion of the bill is usually the largest charge.
In your Explanation of Benefits, the "Provider" indicates whether you have a hospital charge or a professional charge. If the "Provider" is the hospital itself, it's a hospital bill. Anything else is considered a professional charge.
In an itemized bill, hospital charges and professional charges are usually broken down into "hospital" and "professional", or "Hospital Services" and "Physician Services".
Settling a bill with a discount
If a discounted balance is negotiated by Goodbill, the discount is notated internally on the patient's account. The balance will usually remain unchanged in the patient portal, or any paper billing channels, as most discounted offers expire at some point. Therefore - all discounted settlements must be settled over the phone, referencing the agreed discount.
Patients should not wait for their patient portal to update with a new balance, or wait for a new bill. The balance will only update once the discounted amount has been paid via phone, and the billing cycle subsequently refreshed.
Adjustment Time for discounted, paid bills
Once either Goodbill or the patient settles the discounted bill, it takes some time to be reflected on all channels. Hospital billing cycles are a slow-moving machine; once a bill is settled with a discount, then it takes the hospital some time to adjust the balance on all billing channels. It usually takes 2-3 weeks, but can take up to 45 days in some cases. During this time, a patient may still see the full balance in their billing, or the balance minus the discounted settlement.
If, during this time, a patient were to call the hospital to enquire as to why they still had a balance, the hospital would confirm the balance to be zero, and no further payments or needed. It just takes some time for the hospital billing cycle to reflect the settled balance of zero, after the discount. Any collections notices during this time can usually be ignored, until the billing cycle catches up with the adjusted amount.