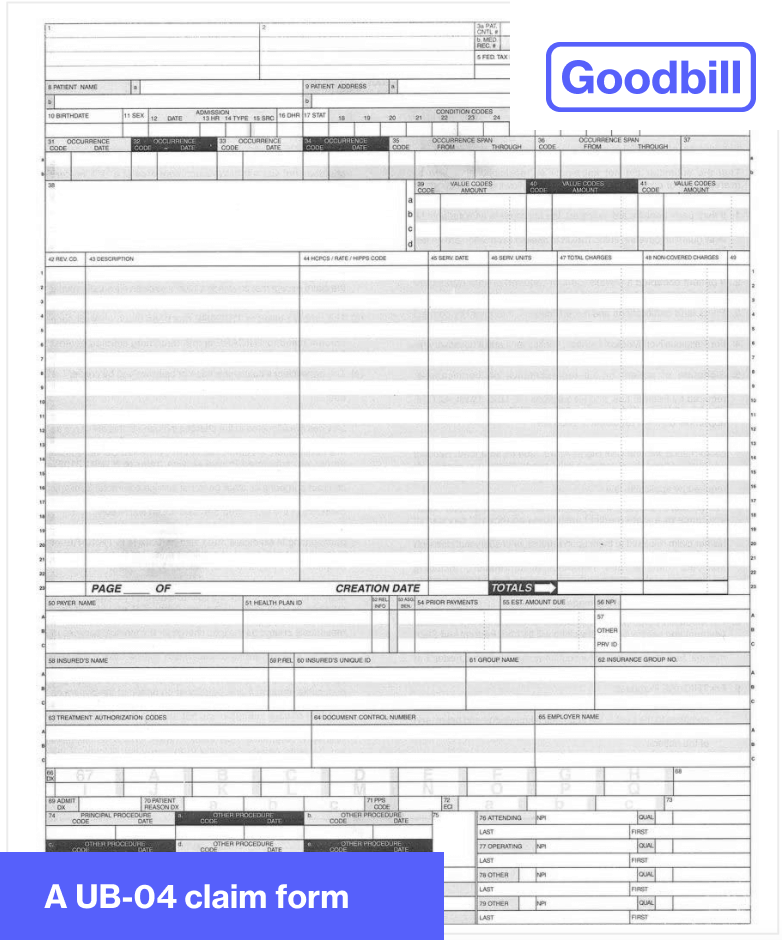
UB-04s - Explained
The UB-04 is a standardized claim form your hospital uses to bill your insurance provider for the procedures you received. It’s generally a single page containing 81 fields, including a line-item breakdown of your procedures, along with CPT, HCPCS, and revenue codes, descriptions, unit quantity and charges.
Goodbill helps you obtain your UB-04 because it gives our medical coding experts an extra layer of detail that itemized bills don’t. For example, it may show CPT “modifiers” that give our medical coders more information to compare against your medical record.
If you were admitted to the hospital, the UB-04 includes diagnosis-related groups (DRGs) that the hospital sends to your insurer. DRGs take into account many factors, including the severity of your condition, as well as the resources your hospital used to treat your condition. Insurance providers use them to reimburse hospitals, as well as understand whether the care you received was fair, and not excessive, to protect them from over-reimbursing a hospital. However, it’s not an exact science, which is where some discrepancies occur: It’s entirely possible for a hospital to assign two patients with the exact same profile different DRGs, where one is more expensive than the other.